27 Aug Eye Diseases
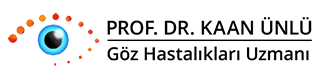
Diabetic Retinopathy:
Diabetic Retinopathy caused by diabetes mellitus is the most common reason for blindness between the age of 20-65. If it is not treated, the risk of blindness is 25 times more than people who don’t have diabetes. The main reason for problems on retina is impairments of retinal vessels due to diabetes. As a result of these impairments; microaneurysms (bubbles in small vessels), bleedings, edema (aggregation of water), exudate (accumulations due to the leakage from the vessels) may be seen on retina at an early stage of disease, and failure to sending adequate oxygen (ischemia) to the neural layer, formation of the new vessels and membranes inside the eyes may be observed at the later stages of the disease.
At the last stage of the disease, blindness may occur as the severe results of bleedings into the eye and separating of the retinal layer from the eyewall (retinal detachment) by the membranes. Therefore, appropriate follow-up, early diagnosis, and treatment are very important. With today’s modern technology, the rate of blindness in these patients can be reduced below %5 percentage.
When patients are diagnosed with diabetes for the first time, they must be examined by an ophthalmologist and they must continue their follow-up examinations with intervals suggested by the physician no more than one year. If an ophthalmologist requires, an eye angiography may be performed during these examinations. This procedure performed while the patient is seating after administrating an iv drug through the armed vessel takes a couple of minutes and with this procedure, the place of the leakage on retina, ischemia, forming of new vessels is examined in detail. Another examination method used frequently is optical coherence tomography (OCT). By this method, it is possible to examine the retinal layer at the 5-10 micron level in seconds.
The main aim of the treatment for diabetic retinopathy is keeping the current vision stable. The most common treatment method for this aim is laser surgery. Laser surgery is a painless intervention. With this intervention, it is aimed to reduce the edema on the retina and to regress the newly formed vessels tending to bleed. In case that laser treatment is not adequate, drugs can be administered into the eye. A surgical operation may be needed in advanced cases. With the vitrectomy operation in which high technology is used and which is performed by an experienced surgeon, bleeding in the eye and membranes are cleaned, and separated retinal layer is replaced. Gas or silicon may be placed into the eye at the end of the operation.
You can see the following videos on this subject:
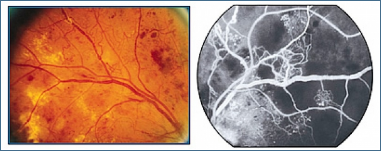
Retinal Tear and Retinal Detachment :
The retina, which is a neural layer which provides vision in the eye is normally fixed to the eyewall. However, vitreous, which is gel-like substance and fills the back of the eye, is weakly adhered to the retina. As result of aging and other diseases, some impairments occur in vitreous and it starts to separate from retina. During this separation, “streak of lights” may be perceived by the patient. At this point of separation, sometimes tears occur in retina. Patients may perceive ‘floaters’ or “shades in front of the eye”.
The liquid that moves through this tear to back of retina starts to separate the retina from the eyewall. This is called retinal detachment with tear. The risk is more in people having myopia, having family background diagnosed with retinal detachment, having undergone cataract surgery, and having retinal detachment in the other eye. However, the reason for retinal detachment without tear which is observed less maybe that membranes occurred in eye pull the contracted retina into the eye (tractional) or fluid (serous) accumulation.
Retinal detachment may cause partial or total vision loss. In the event that tear or weakening and deformation which may cause tears are detected before retinal detachment, laser or cryotherapy are applied around this area. With this procedure, it is aimed to prevent retinal detachment by fixing retinal layer around the tear to the eyewall.
When retinal detachment occurs, it must be treated by surgery as soon as possible.
Delaying the operation reduces the chance of success. During the surgery, depending on the situation of the eye, silicon tapes may adhere to the outer part of the eyewall, gas may be injected into the eye (pneumatic retinopexy) or vitrectomy methods may be used. After vitrectomy, gas or silicon tamponades may be placed into the eye. Recovery of the vision may take a long time, recovery may not occur entirely.
You can see the following videos on this subject:
Age-Related Macular Degeneration (Yellow Spot Disease) :
The macula is the area that provides sharp vision. Cells in this area are damaged in age-related macular degeneration (ARMD), also known as “yellow spot disease” in public, which is among the most common reasons for blindness at later ages (over the age of 60). The most common one is “dry type” in patients and in this type vision loss develops slowly. However, in the “wet type”, which is seen in about %10, vision loss develops quickly. For the treatment of the “wet type” cases, photodynamic treatment or injected drugs called anti-VEGF are used.
You can see the following video on this subject:
Retinopathy of Prematurity:
Retinopathy of Prematurity is characterized by abnormal vasculature and fibrosis development in the retinal layer of premature babies who have born before the development of vessels inside of the eye. Since there is no symptom, babies who have born before 32nd week and under 1500 kg must be examined by an experienced ophthalmologist. Treatment options include follow up, laser, cryotherapy or surgery.
You can see the following videos on this subject:
Cataract :
A cataract is defined as clouding and losing the transparency of the lens. Although it can be seen at any age starting from birth, the most common reason is ‘aging’ of the lens. In cataract, which is accompanied by vision loss as the most important symptom, the only treatment is surgery.
In phacoemulsification, which is known as “seamless surgery” in public, the eye is anesthetized by drops, we reach the inside of the eye through a 2-mm incision and clean the lens with sound waves and put an artificial lens.
You can see the following videos on this subject:
Glaucoma :
Permanent damage on neural layer providing vision occurs in Glaucoma which is one of the most common reasons for blindness. The most important risk factor is high intraocular pressure. However in some glaucoma patients, eye pressure may be at normal levels. Therefore, assessing only the intraocular pressure is not correct to make or exclude the diagnose. In most of the patients, disease follows an insidious pathway, it reduces the visual acuity without causing complaints like pain or redness. Therefore, an early diagnosis is very important. Computer-assisted visual field test, analysis of head of the optic nerve and its fibers are the main methods used for diagnosis and following up the diagnosed patients. Drops to decrease eye pressure, laser or surgical methods are used for the treatment.
You can see the following videos on this subject:
- City and Health Show (03.03.2011) Part : 1/4
- City and Health Show (03.03.2011) Part : 2/4
- City and Health Show (03.03.2011) Part : 3/4
- City and Health Show (03.03.2011) Part : 4/4
Neuro-Ophthalmology:
Neuro-Ophthalmology focuses on visual impairments caused by optic nerve or brain problems as well as movement problems in the eyeball and eyelids. It indicates the methods to reveal, evaluate and treat these problems. Usually, a neurologist and ophthalmologist follow the patient together in these situations. First, a detailed eye examination is needed. If there is a vision or movement disorder that can not be explained by problems inside the eye itself, neurological examination and tomography or magnetic resonance methods might be necessary.
Temporary loss of vision, sudden vision loss, fading of colors, double vision, excessive eyelid opening or drooping, anisocoria (unequal pupil size), contractions of the eyelid and facial muscles may be signs of very serious neurological disorders.
You can see the following videos on this subject:
- City and Health Show (28.04.2011) Part : 1/4
- City and Health Show (28.04.2011) Part : 2/4
- City and Health Show (28.04.2011) Part : 3/4
- City and Health Show (28.04.2011) Part : 4/4
Eyelid Disorders:
Oculoplastic Surgery is a branch that is interested in eyelids, nasolacrimal ducts, and orbita (hole of the eye) diseases. Botox is performed in situations like eyelid introversions (entropium), extroversions (ectropium), droopy eyelids (ptosis), introversion of eyelashes, the opening of congenital or acquired nasolacrimal duct obstructions, operation of eye tumors and eyelid spasm.
The surgical interventions performed to correct sagging eyelids occurred generally due to senility with genetic factors are called blepharoplasty.
Ptosis, known as droopy upper eyelid may be congenital, occur after a trauma and eye operations or muscular weakness due to aging. Droopy eyelid (ptosis) is defined as being at the below normal level of the upper eyelid. In congenital cases, suspenders must be used in order to use frontal muscle and to lift the eyelid. In the case of ptosis at advanced ages, it is aimed to strengthen and shorten the muscle which lifts the eyelid.
The introversion of the eyelids may cause symptoms as abrasion on the surface of the eye, watering, pain, sinking and it may cause wounding on cornea and vision loss at the later stages. This must be is fixed by extroverting the eyelid and eyelashes.
In the situation of facial paralysis or extrovert entropium, the eye is opened to the outer effects. Then firstly dryness occurs and it is followed by infection. Symptoms like watering, sinking, burning may occur. The normal position of the eyelid must be provided again by a surgical operation.
Involuntary Contraction of the Eyelid Muscles (Blepharospasm) :
Blepharospasm, involuntary and excessive contraction of muscles that closes the eyelids, is usually seen after the age of 40. The primary treatment option is botox which is injected into the eyelid and certain areas around it and prevents excessive contraction. The duration of effect of the medication is usually 4 to 6 months. Treatment repetition may be required at regular intervals.
What Is Uveitis?
Uveitis is the inflammation in the vascular layer of the eye. It may recur from time to time after treatment. Iridocyclitis, inflammations that occur in the anterior of the eye, responds early and well to the treatment. Inflammations which are in the posterior of the eye is called “posterior uveitis” and may cause serious, permanent loss of vision.
In most cases, causes that lead to uveitis can not be determined. In some cases, there may be an accompanying rheumatic or infectious disease. These diseases include infectious diseases such as syphilis, tuberculosis, brucellosis, herpes, and AIDS, and systemic diseases like collagen tissue disorders and autoimmune-related disorders. Additionally, Behcet’s disease, sarcoidosis, ankylosing spondylitis, rheumatoid arthritis are common examples of these diseases in Turkey. A detailed evaluation may be required to detect the underlying disease.
Symptoms of uveitis are redness in the eye, sensitivity to light, blurred vision or reduced vision, pain around the eye and floaters. If the disease is located centrally, it is mostly manifested as visual impairment.
Which medications are used in the treatment of uveitis?
When isolated, idiopathic or systemic diseases exist, treatment of uveitis starts after a detailed examination. The treatment of etiology is very important. For example, when uveitis is caused by tuberculosis infection, treatment for tuberculosis infection must be performed with uveitis treatment.
In the treatment of uveitis, usually corticosteroid drops and sometimes pomades are used. Oral or intravenous systemic corticosteroids may be administered, and in some cases, corticosteroid injections may be performed around the eye. Corticosteroids have serious adverse effects and should be discontinued by decreasing gradually. Pupil dilating drops are used to prevent adhesions in the pupil and relieve the pain around the eyes. Immunosuppressants are used alone or in combination with cortisone. Corticosteroid drops, as well as pupil dilating drops, are used to prevent adhesions and relieve the pain around the eyes. Close follow-up and regular controls are substantial in the treatment of the disease.